Welcome to your #Loctorio
A 65-year-old obese male with long-standing type 2 diabetes mellitus presents with shortness of breath and chest pain. The onset of symptoms was gracual over the last 2 days. He describes the chest pain as sharp, stabbing in character, localized to the substerna, midline, and worse with deep inhalation. His past medical history is significant for type 2 diabetes mellitus, diagnosed 20 years ago and managed medically. A review of systems is significant for fatigue, pruritus, and muscle cramps. His lemperature is 38°C (100 4°F), blood pressure is 120/70 mm Hg, pulse is 80/min, respiratory rate is 19/min, and oxygen saturation is 98% on room air. On physical examination, the patient is sitting up and leaning forward. His cardiac exam is significant for a pericardial friction rub. There are crackles over both lung fields bilaterally and dullness to percussion in both lung bases. The abdomen is soft and non-tender Multiple oral aphthous ulcers are present. The skin has a sa low color. Laboratory studies show:
| Serum | |
| Sodium | 136 mEq/L |
| Potassium | 4.2 mEqL |
| Chloride | 106 mEq/L |
| Bicarbonate | 18 mEq/L |
| BUN | 105 mg/dL |
| Creatinine | 3.5 mg/dL |
| Glucose (fasting) | 125 mg/dL |
| Bilirubin, total | 1.2 mg/dL |
| Bilirubin, conjugated | 0.2 mg/dL |
| Uric acid | 25 mg/dL |
| CBC | |
| WBC | 4,500/mm³ |
| Hemoglobin | 14.0 g/dL |
| Platelet count | 275,000/mm³ |
| Urinalysis | |
| Nitrites | Negative |
| Protein | Present |
| Casts | None |
| Crystals | Present (amber birefringent) |
The patient’s chest X-ray shows evidence of bilateral pleural effusions (left greater than right). The ECG is shown (click on the image to enlarge). Transthoracic echocardiography (TTE) reveals a small pericardial effusion. Which of the following is the best course of treatment for this patient? 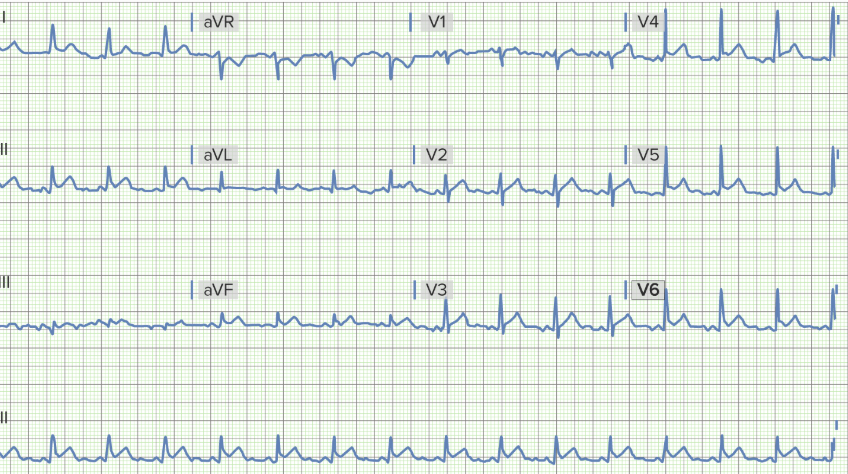
A 65-year-old man presents with dizziness, shortness of breath, and palpitations. The symptoms began approximately 3 hours ago and have not improved, he feels "heart racing" and dizziness when standing. His past medical and surgical history are significant for a left anterior descending STEMI two weeks ago, followed by a coronary artery bypass graft (CABG). Current medications are aspirin (81 mg orally daily), rosuvastatin (20 mg orally daily), and enalapril (10 mg orally twice daily). Vital signs are temperature 37°C (98.6°F), blood pressure 105/70 mm Hg, pulse 135/min, respirations 16/min, and oxygen saturation 97% on room air. On physical exam, the patient is alert and cooperative. The cardiac exam is significant for tachycardia and an irregularly irregular rhythm. There are a few basilar crackles in the lungs. The abdomen is soft and non-tender with no hepatosplenomegaly. There is trace bilateral pitting edema in the ankles. Laboratory tests are significant for:
.tg th{border-color:black;border-style:solid;border-width:1px;font-family:Arial, sans-serif;font-size:14px; font-weight:normal;overflow:hidden;padding:10px 5px;word-break:normal;} .tg .tg-0pky{border-color:inherit;text-align:left;vertical-align:top}
A 63-year-old woman with end-stage renal disease complains of feeling lightheaded for the past month after hemodialysis. She worries she might lose her balance and fall. She has had diabetes mellitus for 22 years. Her medications include folic acid, vitamin B12, amlodipine, and erythropoietin. At the clinic, her blood pressure is 135/80 mm Hg when lying down before dialysis and 110/55 mm Hg when seated after hemodialysis. Cardiopulmonary examination shows no abnormal findings. Laboratory studies after hemodialysis show a Hb of 10.5 mg/dL, blood glucose of 189 mg/dL, and a hemoglobin A1C of 7.1%. To reduce the likelihood of falls, what is the most appropriate management?
A 24-hour-old girl is found to be cyanotic in the newborn nursery. She was born via spontaneous vaginal delivery at 38 weeks' gestation to a gravida 1, para 0 healthy mother who received routine prenatal care. The patient is small for her gestational age. She has lower-extremity cyanosis along with a mesh-like mass on the back of her neck. Her pulse is 150/min, and respirations are 48/min. Blood pressure is 120/80 mm Hg in the right arm, 124/82 mm Hg in the left arm, 80/40 mm Hg in the right leg, and 85/45 mm Hg in the left leg. Femoral pulses are 1+ and delayed. A cardiac examination shows a continuous murmur in the interscapular area. Auscultation of the lung reveals faint crackles at the base of the lung fields bilaterally. Which of the following is the most appropriate next step in management?
A 57-year-old man presents to the emergency department for evaluation of slurred speech and left arm and leg weakness over the last 3 hours. History reveals hypertension that is being treated with hydrochlorothiazide. Vital signs include: blood pressure of 110/70 mm Hg, heart rate. 104/min, respiratory rate 18/min, and temperature 36.6°C (98.0°F). Physical examination reveals 2/5 strength in both the left upper and lower extremities. After 2 hours, the patient's symptoms suddenly disappear. An electrocardiogram (ECG) shows atrial fibrillation. Which of the following medications could prevent ischemic attacks in this patient in the future?